Support with Antibiotics
Antibiotics = Gut Destruction
You should only take an antibiotic when it is necessary. As rarely as possible, but as often as needed. It is important that antibiotics are only taken if you have a pathogenic bacterial infection (antibiotics are ineffective for infections with viruses and fungi). Your doctor can easily determine this in a laboratory.
For common colds with a moderate cough, runny nose or sore throat, antibiotics are not usually necessary and should not be prescribed just in case. With conditions such as sinusitis, tonsillitis or urinary tract infections, an antibiotic is sometimes necessary - however, serious infections, such as pneumonia triggered by bacteria or a kidney infection, must be treated with an antibiotic. Whenever antibiotics are taken, it is important that the intestines are supported with sufficient good bacteria that occur naturally in the human intestine. Supplementing good gut bacteria in sufficient quantities is also a crucial factor here: Probiotic bacteria are most effective in the 24 hours after they are activated. In the case of yoghurts, this activation stage happens in the dairy, and by the time the yoghurt from the grocery shop has found its way into your fridge, there are hardly any living bacteria left. With probiotics in powder form, however, the bacteria are activated outside your body - just before you want to send "reinforcements" to your gut. Thus, a sufficient number of viable and reproducing bacteria arrive in your intestine.
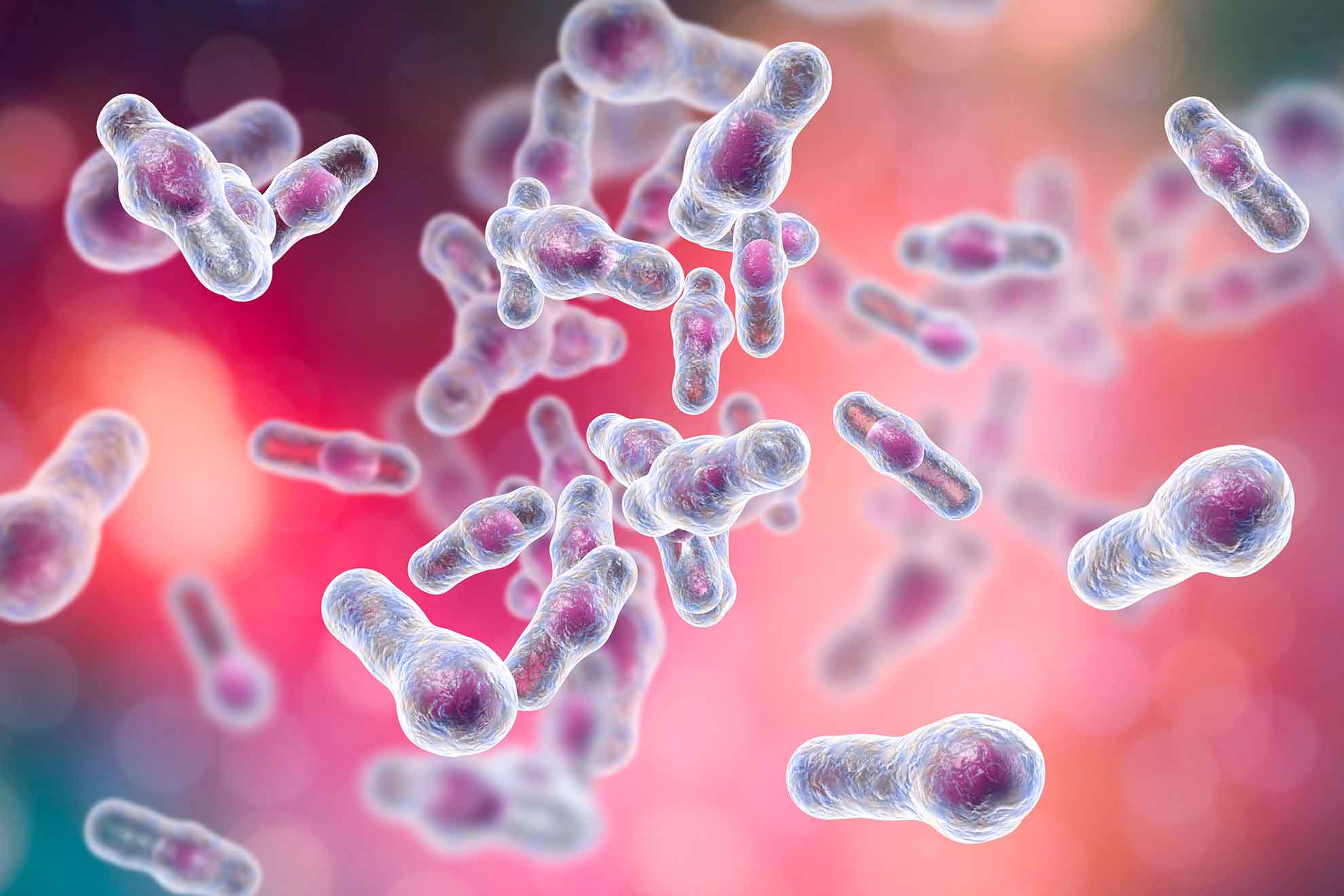
Clostridium difficile
All-round Antibiotics?
Depending on the active substance used, antibiotics can cause diarrhoea in up to 50% of applicators. However, diarrhoea is not always directly associated with the medication, because these adverse effects can also occur even weeks after finishing the antibiotic treatment. But how can antibiotics cause diarrhoea? The main problem is that antibiotics cannot distinguish between "good" and "bad" bacteria and thus cause a complete destroy of all kinds of bacteria in their path - even the beneficial intestinal flora is massively damaged and inflammation of the intestinal mucosa occurs. The damage caused to our intestinal flora means that our natural "defence" mechanism is also weakened. Aggressive, disease-causing germs, which are also resistant to antibiotics, can therefore multiply almost unhindered. The bacteria "Clostridium difficile" often takes over the intestine and leads to problems here. Up to 20 % of antibiotic-associated diarrhoea (AAD) is caused by this harmful bacterium - in technical jargon, this is called Clostridium difficile-associated diarrhoea (CDAD).

What are the symptoms of diarrhoea caused by antibiotics?
Diarrhoea is when you have more than 3 bowel movements a day, the stool is very soft to liquid and the amount of stool has increased significantly. This is often accompanied by cramping abdominal pain, flatulence, nausea and vomiting. These symptoms can occur immediately or even several weeks after starting the course of antibiotics. If you experience side effects, it is important not to stop taking the prescribed antibiotics without consulting your doctor: This is because unwanted, dangerous germs may then survive and develop resistance to antibiotics.
When is it necessary to consult a doctor when taking antibiotics?
- If diarrhoea occurs over the course of taking antibiotics and lasts longer than 2 weeks
- With babies, small children or old people affected by severe diarrhoea.
- If diarrhoea is accompanied by high fever, dizziness, extreme weakness or severe, prolonged abdominal cramps.
- If there is a risk of dehydration: not enough fluid can be taken in, the urine is noticeably dark in colour or the amount of urine decreases sharply.
- If stool is extremely dark in colour ("tarry stools") or contains blood, mucus or pus.
„Three things change our gut flora in a particularly negative way: poor diet, stress and - the administration of antibiotics."
Probiotics for Diarrhoea
We need probiotic bacteria in high numbers in our gut, as only they can ensure that our body can process the food we eat correctly. If the diversity of the gut flora is reduced by taking medication, then the fermentation or putrefaction processes begin, which influence the intestinal activity or also lead to increased fluid excretion and, through toxins, to increased permeability of the damaged intestinal mucosa. Probiotics with highly active bacterial strains can lead to a normalisation of stool frequency, regeneration of the damaged intestinal mucosa and an improvement in stool consistency. Stress, which promotes the peristalsis in the gut and additionally has a harmful influence on the balance in the intestine, should be avoided. Diarrhoea is often a symptom of irritable bowel syndrome, which is triggered among other things by stress.
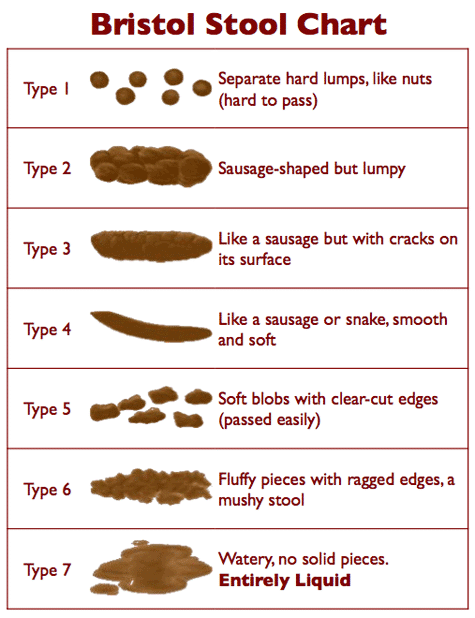
Bristol Stool Chart
Type 5, 6, 7 shows the typical forms of stool in the case of diarrhoea